Family-centered therapy creates positive outcomes for a child with a neuromotor impairment (such as cerebral palsy) through the partnership created between the family of a child with a disability and the therapy professional. Together, they get the child's home exercise done. If not done -- with good form and in appropriate intensity and duration -- benefit is less likely.
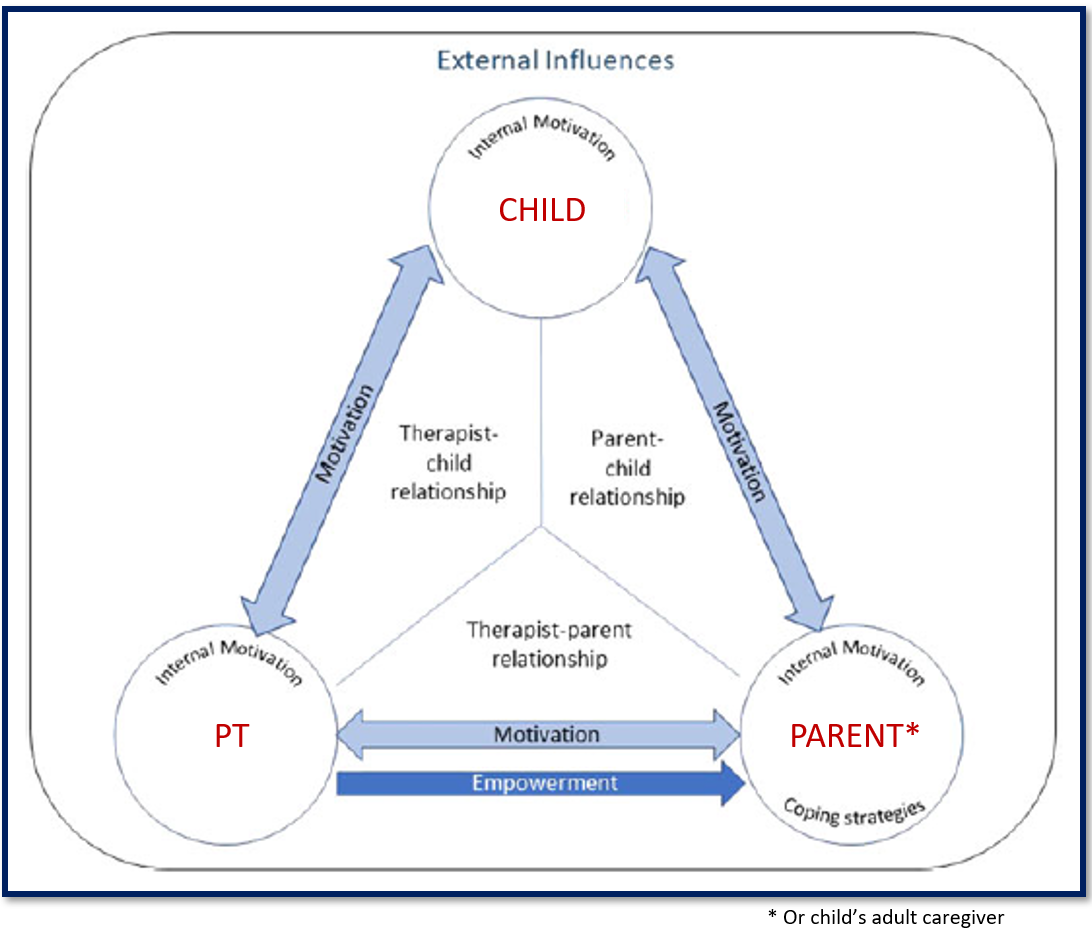
The priorities and motivations of three parties have to align for there to be good compliance with a home exercise program: The child who is receiving therapy, the parent or other adult caregiver who structures the child’s environment, and the PT who recommends the content of the exercise program based on clinical knowledge. Together, they form a “compliance triangle.”
Relationship-Driven, Family-Centered Care via TelePT: Reflections in the Wake of COVID-19
In response to the throttling of children’s therapy programs precipitated by COVID-19 shutdowns, interest in the use of telehealth has increased among service providers at both the clinical and administrative levels. TelePT promises to be particularly appropriate in devising programs of on-going, therapeutic exercise interventions for children with neuromotor disorders. From the lay perspective, physical/physio-therapy (PT) which is seemingly characterized by the "hands-on," and corrective approach to managing impairments, makes a counter-intuitive candidate for delivery over telehealth. Over the past decades, however, PT as a discipline has increasingly adhered to a relationship-driven, family-centered model of intervention. This model is "hands-off," figuratively if not always literally and hence is not necessarily disconsonant with delivery mediated by telehealth technology.
On November 30, 2022, the RERC-DC published an article in Frontiers in Psychology that explores in depth the experiences and reflections of seven practicing therapists, on the impact of telehealth, telePT on the operationalization of relationship-based, family-centered methods into therapy. Results identified eight principal themes emerging from participants’ descriptions of their experience of delivering therapy over telePT. Four of these themes correspond to the tenets of relationship-driven, family-centered care identified across four frameworks applied to pediatric rehabilitation. The remaining four themes focus on the particularities of the telePT modality and its viability in clinical practice. The ability telePT afforded to “see into the child’s environment,” emerged arguably as the greatest value of the modality in patient care. It revealed to therapists so much that they didn’t know about their patients’ progress and, more strikingly, had not realized they didn’t know. TelePT provides a unique window into the child’s functioning in the hours he is not in therapy. Given its potential in parent-therapist relationship building, assuring the ecological validity of therapy programs and the empowerment of families who seek it, telePT is likely to be part of the future of PT and one driver of its evolution as a profession. There is a compelling case to retain telePT modalities offering them alongside in-person formats for convenience, safety, and service quality enhancement.
Read the full text of the article HERE.
Doing Therapy at Home
Part 3 of a symposium the RERC-DC conducted at the American Congress of Rehabilitation Medicine's annual conference in Chicago, IL, November 11, 2022, focused on family-centered care in the context of PedBot Home research and lessons learned from the shift to providing services via telehealth precipitated by COVID-19. You can download and view the slides here. Part 3 starts on slide 48.