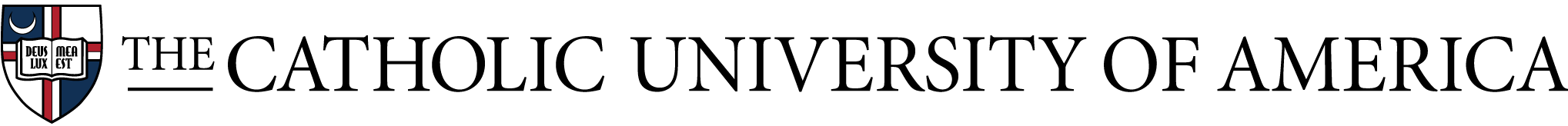
Infants grasping HUGS-1,-2 tethered, wired toy bar (l) and untethered, wireless HUGS-3 toy (r).
Executive Summary
In this project, we are exploring a family-centered, home-based approach to objectively and quantitatively assess the development of hand grasp in infants at risk for fine motor delay, and predict the future diagnosis of delay. Undiagnosed motor delay can prevent the timely use of early interventions, and lead to motor disabilities throughout life. Through biweekly in-home assessments administered by the infants’ parents/caregivers, we are learning about the development of spontaneous hand use in infants 12-52 weeks of age through 3D video capture, while at the same time measuring their interactive grasp force with a specially instrumented toy: the Hand Use and Grasp Sensor (HUGS) system.
Fourteen infant-caregiver pairs advised us during the initial phase of HUGS design and development in 2019-2020 to ensure that both the toy and the process for deploying it to collect infant grasp data were optimized for home use. HUGS provides biofeedback of the infant’s own grasp force through different sensory channels, including touch (vibration), vision (lights), and hearing (sounds), to learn whether each infant is able to integrate sensory feedback into an adaptive hand grasp. This information could signal potential avenues for early interventions to encourage object exploration and functional hand use.
We did not, however, find any difference in infant grasp variables (ex., force, duration) based on sensory feedback, though we did find that infant grasp increases in force, duration, and frequency as the infant gets older. We also found that the size and shape of toys influenced the magnitude of infant grasp force variables with bar-shaped toys providing a better opportunity to expose grasp performance than ball-shaped toys. See "Hand Use and Grasp Sensor System in Monitoring Infant Fine Motor Development."
The most common neuromotor disorder of childhood, cerebral palsy, may be diagnosed early in infancy via clinical video review of the child using a protocol known as the General Movements Assessment (GMA). We leveraged GMA kinematic features to analyze the upper limb movement of eight infants from video captured when they were three, four, and five months old. Subsequently, we compared outcome metrics against the clinical evaluations of the videos by clinicians with expertise in pediatric neurology and physiatry demonstrating that certain GMA metrics may be useful in identifying neuromotor delay with a sole focus on the upper limbs of a seated infant. See "Characterization of Infants' General Movements Using a Commercial RGB-Depth Sensor and a Deep Neural Network Tracking Processing Tool: An Exploratory Study."
HUGS was redesigned as HUGS-2 implementing ease-of-use criteria identified by families during the first phase of the study. These criteria became all-important to support autonomous use of the HUGS system by family during the COVID-19 lockdown. See "Evolution of a System to Monitor Infant Neuromotor Development in the Home: Lessons from COVID-19."
The next phase of HUGS design and testing (HUGS-3) moves sensor technology implementation from a wired, stationary data collection toy frame to a wireless (Bluetooth Low Energy) handheld grasp sensor controlled by an app on the parent/caregiver's smartphone. Follow our work as we develop and test HUGS-3 (2022-2023) at our development and learning site: HUGS-Lab.org.
Expected Deliverables
Threefold: (1) the Hand Use and Grasp Sensor (HUGS) system, a home-based assessment tool for infant grasp development, (2) typically developing norms for the HUGS system, and (3) software to use HUGS outcomes to predict fine motor delay at 1 year of age in at-risk infants.
Meet the HUGS Team
-
Manon Maitland Schladen, PhD
Learn More -

Peter Lum, PhD
Learn More -
Lin-Ching Chang, DSc
Learn More -

Olga Morozova, MD
Learn More -

Ugo Della Croce, PhD
Learn More -

Sahana Kukke, PhD
Learn More